The Approach to the Poisoned Patient
- 12 feb 2021
- 17 Min. de lectura
Overview
Most toxicologic exposures involve ingestions or localized chemical/biologic exposures involving single individuals with limited risk to medical personnel. In the uncommon event of an exposure which could be transmitted to emergency personnel, be sure to perform decontamination FIRST and OUTSIDE of the Emergency Department in order to not contaminate your personnel or life-saving equipment. At a minimum, the readily available PPE (cap, gown, gloves, mask, and eye protection) should be worn by all personnel in order to prevent accidental exposure.
As with all unstable patients, the initial assessment (once safe) begins with the ABCs. A detailed history and physical examination is key. Knowledge of medications, medical problems, and potential ingestions or exposures are very important historical facts in order to narrow down the list of potential toxic agents.
The physical exam should be comprehensive with special attention directed at finding evidence of a specific toxidrome. Also be wary of anchoring on the diagnosis of toxin exposure: don’t forget to keep trauma, CNS infection, and the myriad of other causes of altered mental status on the differential.
Also don’t forget the generally harmless “quick fix” medications that can rapidly reverse altered mental status in a previously comatose patient – naloxone and dextrose. Generally, patients will not be harmed with the indiscriminate provision of sugar and opioid reversal… though care should be taken in the chronic opioid abuser: lower doses are probably better such as 0.04-0.1mg IV at a time.
There are many, many reasons why drugs become toxic so remember that not all patients did something nefarious… many things affect drug clearance/protein binding/metabolism including underlying renal disease, hepatic dysfunction, dietary changes, iatrogenic, etc.

General approach
ABCDE approach in poisoned patient
A airway
Airway protection is a maximum priority in poisoned patients, as some of them can suffer from decreased level of consciousness and vomits
The initial priorities for a poisoned patient presented to the emergency department are: securing the airway and breathing and stabilizing the circulation. Adequate ventilation and intubation with mechanical ventilation must be done early in the intoxicated patients with depressed mental status, except in cases of easy reversible causes of coma like opioid intoxication or hypoglycemia to prevent complications of intubation like aspiration. Other indications for intubation include severe acid-base disturbances or acute respiratory failure. In intubated patients, development of a respiratory acidosis must be prevented by adequate ventilation; in some cases like high-grade physiologic stimulation, the patient may need sedation and paralysis to prevent complications such as hyperthermia, acidosis, and rhabdomyolysis.
B breath
Most of the poisoned patients will require ventilatory support after having protected the airway, it's important to monitor O2 sat and caphnography .
C circulation
The resus medication is similar to other critical patients, we have to add antidotes and practice the CPR at least 120 minutes in patients exposed to cardio toxic agents.
Hypotension Drugs cause hypotension by four major mechanisms: decreased peripheral vascular resistance, decreased myocardial contractility, dysrhythmias, and depletion of intravascular volume. First-line treatment of hypotension is IV fluid bolus (10 to 20 mL/kg); if hypotension is not responding to fluid, it may be necessary to add vasopressors such norepinephrine. Norepinephrine is better than dopamine.
Hypertension Elevated blood pursues caused by CNS sympathetic overactivity, increased myocardial contractility or increased peripheral vascular resistance, or a combination. The treatment of hypertension and agitated patients starts with sedatives such as benzodiazepines; if not responding for initial treatment and there is evidence of end-organ dysfunction, calcium-channel blocker is preferred treatment. The use of beta-blockers is not recommended in the case of sympathetic hyperactivity because it may cause unopposed alpha-adrenergic stimulation and intensified vasoconstriction.
D disability
There are different agents that can decrease the level of consciousness or cause altered mental status, sedation can be indicated
The best treatment of intoxicated patients with seizures is benzodiazepines; we may add barbiturates if necessary. Phenytoin is not recommended to control seizures in poisoned patients.
E exposure
This item won't change. The patient should be exposed and search for bruises, punction signs or trauma signs etc.
Initial orders
VS (hyper and hypotension already explained in C of ABCDE approach)
Elevated temperature (hyperthermia) due to drug toxicity (e.g., sympathomimetic overdose, serotonin syndrome, or neuroleptic malignant syndrome) must be treated aggressively to prevent complications like rhabdomyolysis, organ failure, and disseminated intravascular coagulation. Treatment of hyperthermia includes active cooling like ice water immersion; if active cooling is ineffective, the patient may need sedation, neuromuscular paralysis, and intubation.
Laboratory tests
Full laboratory panels should be drawn, especially electrolytes, serum osmolarity, hepatic function, coags, urine beta HCG, aspirin, tylenol, ethanol, and any other specific levels based on your history and physical exam.
Blood test must be done with all intoxicated patients; especially in the case of intentional overdose, the laboratory test should include basic lab (full cell count and kidney function liver function and electrolytes). Acetaminophen screening is very important in every patient presenting with altered mental status or intentional overdose [8].
For the patients with an acid-base abnormality, serum osmolarity needs to be checked, looking for increasing osmolar gap, which rolls out toxic alcohol ingestion.
In the case of presence of anion gap, metabolic acidosis may help and give to physician a clue of ingestion of certain toxins like (salicylates, ethylene glycol, and methanol or other drugs which may cause high anion gap metabolic acidosis; also serum creatinine, glucose, ketones, and lactate should be tested to detect other causes of the anion gap acidosis.
When serum creatinine is elevated with a normal BUN, this finding is seen in the case of isopropyl alcohol toxicity (or with diabetic ketoacidosis). Co-oximetry can be used for rapid diagnosis of carbon monoxide toxicity and methemoglobinemia.
Toxicology screening is not necessary in case of nonintentional ingestion are asymptomatic patient or have clinical findings that are match with the medical history.
Drugs of abuse to opioids, benzodiazepines, cocaine metabolites, barbiturates, tricyclic antidepressants, tetrahydrocannabinol, and phencyclidine can be detected by using immunoassay screens in urine.
Positive and negative screens for drugs do not necessarily confirm diagnosis of acute poisoning but require further investigations.
EKG
An EKG is a must in all unknown toxic exposures, as interval derangements and electrocardiographic clues to underlying toxicities are very common.
ECG should be done on all patients who are symptomatic or who have been exposed to cardiotoxic agents looking for the rate and conduction; ECG abnormalities may help in diagnosis or may help as prognostic information. Specific attention should be paid to QRS interval and QT interval; in the case of prolongation of QT or QRS sodium bicarbonate infusion should be strongly considered.
EKG abnormalities
- Prolonged QT interval
. Antihistamine: astemizol, difenidramine, loratadine, terfenadine
- Antibiotics: claritromicin, quinolones
- Antipsichotics: clorpromazin, droperidol, haloperidol, quetiapine, risperidone, tioridazine
- Arrhythmical: quinidine, procainamide, flecainide, propanerone, amiodarone, sotalol
- Antidepressants : venlafaxine, citalopram
- Others : metadone, cloroquine, cisapride, tacrolimus, pentamidine
- wide QRS
Amantadine, carbamacepin, cloroquine, disopiramide, procainamide, citalopram, cocain, TCA, flecainide, difenidramine, propanolol, verapamil
- toxic bradycardia
Calcium channel blockers
Beta blockers
Digoxin
Acetil cholinesterase inhibitors
Myocardial depression, peripheral vasodilatation, AV conduction abnormalities
Ventricular tachycardia occurs because of tricyclic antidepressant toxicity. Sodium bicarbonate is first line therapy. Types IA (e.g., procainamide), IC, and III antiarrhythmic agents may worsen cardiac conduction; hence, they are not recommended; also, using these agents could be potentially dangerous. Magnesium sulfate can also be used in the case of drug-induced torsade de pointes and prolonged QT intervals on ECG. Digoxin toxicity with life-threatening tachyarrhythmias or bradyarrhythmias should be treated with specific Fab fragments (Digibind).
Bradyarrhythmias Treatment of bradyarrhythmias with hypotension starts with atropine and/or temporary pacing. Calcium, glucagon, or high-dose insulin are used in the case of calcium channel blocker or beta blocker intoxication.
Radiographic studies
Imaging with a chest Xray can be helpful in assessing for pulmonary edema, pill fragments, or other radiopaque objects in the chest or abdomen.
Imaging examinations are not necessary in every poisoned patient but may be useful in some situations where the toxins are radiopaque [6]. The toxins which are radiopaque can be summarized by the mnemonic “CHIPES”. also, “body packers” may be seen on plain films . Chest x-ray is useful in the case of noncardiogenic pulmonary edema and the acute respiratory distress syndrome due to exposure to certain toxins.
Body Packers and Stuffers
Body stuffer – Spontaneous ingestion of poorly packaged drugs, for instance swallowing a bag of contraband just prior to arrest.
Likely will not require whole bowel irrigation, usually admitted for observation for 24 hours though some suggest 6 hour observation period and then discharge if no evidence of toxidrome.
Body packer – “Drug mule,” a carefully planned ingestion of presumably carefully packaged illicit drugs.
If asymptomatic but known packer, can CT scan to quantify packets, or just give AC and WBI until several clear stools without packets.
If second CT scan at this point is negative, then they are clear (if they remain asymptomatic).
If known or suspected cocaine packing and the patient is symptomatic, i.e. sympathomimetic toxidrome; highly likely one of the packets has burst or is leaking, which is an indication for emergent surgery.

After the ABCDE approach our next step will change depending on GCS
8 or less
"coma cocktail" Vitamine B1, glucose, naloxone, flumazenil
If neurological focal deficits Cranial CT
GCS more than 8
- decrease absorption
- antidotes
Secondary evaluation and approach
Decontamination
Coma and Seizure treatment
Antidotes
Increase excretion
History taking
History of the present illness is very important and can be obtained from the patients if they are alert and conscious; although the history following intentional ingestion is often unreliable, which makes history taking very challenging especially if the patients are comatose or cannot give their history, in such situations, history can be taken from collateral information from family, friends, ambulance crew, or medical records looking for past psychiatry illness, previous history of suicide or drug abuse, chronic medication, etc.
History must include time, route of entry, quantity, intentional or accidental exposure, availability of drugs at home, and if any member of the family has chronic diseases (hypertension, diabetic, etc.) and missing tablets or any empty pill bottles or other material was found around him [4]. It is very important to ask specifically about the use of traditional or herbal remedies and dietary supplements.
Physical examination (In secondary Survey)
Physical examination of poisoned patients may give clues regarding the substance which has been abused and toxidromes. Physical examination includes: general appearance,
Mental status (agitated or confused) Some drugs or substances affect the central nervous system either causing agitation or depression. Central nervous system depression may be caused by the following: Anticholinergics, antidepressants, antipsychotics, lithium, cholinergic beta blockers, clonidine, and sedative-hypnotics. Central nervous system agitation Sympathomimetics, anticholinergics, salicylates, central hallucinogens, drug withdrawal states, carbon monoxide, hypoglycemic agents, and heavy metals.
Skin (cyanosis, flashing, and physical signs of intravenous drug abuse (track marks) Red and flushed skin occurs in the case of overdose of anticholinergic agents, antihistamines, TCAs, atropine, scopolamine, and phenothiazines. Pale and diaphoretic skin occurs in the case of sympathomimetics (cocaine), cholinergic agents (organophosphates), central hallucinogens (lysergic acid diethylamide (LSD) and phencyclidine) and salicylate toxicities. Cyanotic skin occurs in the case of methemoglobinemia and sulfhemoglobinemia.
Eye examination: (pupil size reactivity lacrimation and nystagmus) Common drugs causing miosis
Opioids (morphine, hydromorphone, and oxycodone)
Sedative-hypnotics (barbiturates and benzodiazepines)
Cholinergic (nerve agents and organophosphate insecticides)
Sympatholytic (clonidine and oxymetazoline)
Common drugs causing mydriasis
Sympathomimetics (cocaine and caffeine)
Anticholinergics (atropine, scopolamine, and TCAs)
Hallucinogens (LSD, mescaline, and psilocybin)
Serotonin syndrome
Common drugs causing nystagmus
Barbiturates, carbamazepine, phencyclidine, phenytoin, and lithium
Odor (garlic, bitter almonds, glue, alcohol, etc. (Table 1).
Oropharynx hyper salivation or dryness;
Chest: breath sound, bronchorrhea, wheezing, heart rate, and rhythm regularity;
Abdomen examination (bowel sound, tenderness, and rigidity);
Limbs (tremors and fasciculation), patient’s clothing (looking for any medications and illegal drugs) [3].
Toxidromes
The term toxidrome was coined in 1970 by Mofenson and Greensher. Toxidromes are a group of abnormal physical examinations and abnormal vital signs known to be present with a specific group of medications or substances. The most common toxidromes are cholinergics, anticholinergics, sympathomimetics, opioids, and serotonin syndrome [4, 5].
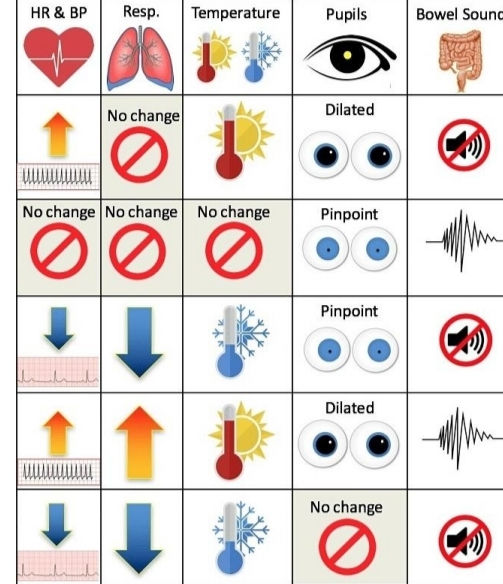
ANTICHOLINERGIC
CHOLINERGIC
OPIOID
SYMPATHOMIMETIC
HIPNOTIC/SEDATIVE
Anticholinergic – The old mnemonic rules supreme here – blind as a bat (mydriasis), mad as a hatter (altered mental status), hot as Hades (hyperthermic), red as a beet (flushing), dry as a bone (no sweating), the bowel and bladder increase their tone (urinary retention, decreased bowel sounds), and the heart runs alone (tachycardia).
Commonly described symptoms
Lilliputian hallucinations (picking at unseen small objects on the body), “pleasantly altered.”
Synesthesia – crossed sensory stimuli such as “I can taste the music.”
Common offending agents (many)
Over-the-counter medicines such as antihistamines
Synthetic cannabinoids like spice
Antipsychotics, antidepressants, antiparkinsonian drugs, antiemetics (phenothiazines), muscle relaxants (cyclobenzaprine)
Differentiate from sympathomimetic toxidrome by:
Dry skin
Mydriasis with limited or absent pupillary response to light
In anticholinergic toxidrome there is inhibition of cholinergic input to the ciliary apparatus of the eye; therefore, pupillary response to light will be limited or absent, whereas the opposite is true in the sympathomimetic toxidrome.
Sympathomimetic
Agents – Cocaine, MDMA (ecstasy), ephedrine, methamphetamine, khat, etc.
Toxidrome – Hypertension, tachycardia, diaphoresis, mydriasis, hyperthermia, CNS excitation and delirium.
Differentiate from anticholinergic toxidrome by diaphoresis and mydriasis with brisk pupillary response.
Treatment – Benzodiazepines are the mainstay of treatment in the patient suspected of a sympathomimetic ingestion/toxicity. Benzodiazepines restore inhibitory balance to the CNS to help prevent the tremendous sympathetic outflow stimulated by these agents. Life-threatening hyperthermia may also occur; aggressive cooling measures and benzodiazepine administration are keys to early treatment.
For refractory hypertension, consider phentolamine (pure alpha blocker).
Be wary of mixed alpha/beta antagonist drugs such as labetalol as the alpha:beta ratio is very much in favor of beta blockade, approx. 1:7 ratio. Efficient beta blockade of beta-2 receptors will worsen vasoconstriction, causing nearly unopposed alpha-agonism by the original toxic agent leading to worsening hypertension.
Beware dysrhythmias: SVT is common and sodium channel blockade often leads to wide complex tachycardia that may degenerate into non-perfusing rhythms.
SVT unresponsive to benzodiazepines and cooling can be treated with calcium channel blockade.
Wide complex tachyarrhythmia, especially in cocaine toxicity, should be treated with empiric bicarbonate bolus and ACLS measures.
Opioids
Agents: Long/short acting opioids, heroin, methadone, buprenorphine, etc.
Toxidrome – Drowsy, hypoventilation, hypotension, apnea, miosis, decreased bowel sounds.
Treatment – Largely supportive (airway support, fluids, vasopressors), if acute overdose can use naloxone in higher doses (0.4-2mg IV).
Caution in the chronic opioid dependent patient or opioid abuser as may precipitate withdrawal, also the patient will become agitated and combative if completely reversed immediately so should start with lower doses of repeat aliquots of 0.04-0.2mg IV.
Generally the goal is to find the amount required to reverse the respiratory depression and allow spontaneous respiration: the total dose given to reach this goal should be multiplied by 2/3, and this amount given as a drip per hour. Obviously the patient needs to be monitored but in a strict opioid overdose without other factors, reversal of respiratory depression is the most important step.
Sedative/Hypnotic
Agents: Barbiturates, benzodiazepines, alcohol, GHB, sleep aids, zolpidem, buspirone.
Toxidrome – Drowsy, slurred speech, nystagmus, hypotension, ataxia, coma, respiratory depression.
Treatment is supportive, intubation as necessary for airway control, fluids/vasopressors for hypotension. Few specific antidotes, flumazenil is antidote for benzodiazepine overdose but should almost never be used… unless it is a known iatrogenic overdose of a pure benzodiazepine without any possible stimulant medication in a person that is not a chronic user of benzodiazepines nor has a history of seizures. Otherwise, may cause seizures refractory to benzodiazepine administration.
***Please see http://www.emdocs.net/wp-content/uploads/2014/10/Flumazenil-Bodford-.pdf for further details.***
Cholinergic
Agents – Organophosphate and carbamate pesticides, nerve agents; mechanism is poisoning of acetyl cholinesterase at ganglionic and neuromuscular junctions leading to increased acetylcholine neurotransmitter stimulation, with both muscarinic and nicotinic receptor stimulation effects.
Toxidrome – DUMBBELLS (Diarrhea/Diaphoresis, Urination, Miosis, Bradycardia, Bronchorrhea, Emesis, Lacrimation, Low BP, Salivation).
Killer B’s (from muscarinic stimulation) – Bradycardia, Bronchorrhea, Bronchospasm.
Will also get nicotinic stimulation effects such as fasciculations, tetany, paralysis and increased sympathetic ganglionic stimulation which may result in paradoxical tachycardia and hypertension early.
Seizures are common in overdose.
Treatment – These patients will commonly need prehospital decontamination, DO NOT bring into the ED until they have been adequately decontaminated. The most common cause of death is airway compromise so early securing of the airway is paramount.
Atropine in high doses of 2-4mg IV at a time, keep giving until oral secretions are dry.
Pralidoxime (2-PAM) in order to reverse acetyl cholinesterase inhibition. This must be given early before enzyme “aging.”
Benzodiazepines for seizures and agitation.
Other syndromes
Serotonin syndrome
Patients present with altered mental status, hypertensive, and tachycardia, myoclonus, hyperreflexia, hyperthermia, and increase in muscle rigidity. Most common causes: SSRI interaction or overdose of SSRIs.
MAOIs, tricyclic antidepressants, amphetamines, and fentanyl [4].
Hallucinogenics Patients present with hallucinations, perceptual distortions, depersonalization, synaesthesia, and agitation. Mydriasis, hyperthermia, tachycardia, hypertension, tachypnoea, and nystagmus. Most common causes: phencyclidine, LSD, mescaline, psilocybin, and MDMA [“Ecstasy”].
Ethanolic Patients present with central nervous system depression, ataxia, dysarthria, and odor of ethanol.
Extrapyramidal Patients present with dystonia, torticollis, muscle rigidity, choreoathetosis, hyperreflexia, and sometimes seizures. Most common causes: risperidone, haloperidol, and phenothiazines.
Salicylate Patients with salicylate toxidrome present with altered mental status, mix respiratory alkalosis, metabolic acidosis, tinnitus, tachypnoea, tachycardia, diaphoresis, nausea, vomiting, and hyperpyrexia. Most common toxin: aspirin and oil of wintergreen (methyl salicylate).
Clinical approach
Breefing (role asingment)
Primary Survey ABCDE approach
History takning (by any other member of the team)
Secondary survey.
Gross decontamination
Patient must be fully undressed and washed thoroughly with copious amount of water twice regardless of how much time has elapsed since the exposure. All the clothing must be removed and placed in plastic bags, and then the bags must be sealed; no need to neutralize an acid with a base or a base with an acid because that may lead to more tissue damage because the heat could be generated by this reaction. Using any greases or creams must be avoided because they will only keep the xenobiotic in close contact with the skin and ultimately make its removal more difficult.
Decontamination must be done in an isolated specific area. Gross decontamination is used in chemical, biological, and radiation exposure. Healthcare providers must wear universal precautions (gown, gloves, and sometimes may need personal protective equipment.
Ocular decontamination
In the case of eye exposures to chemical substance, initially, application of a local anesthetic agent (e.g., 0.5% tetracaine) may be needed, then copious irrigation with crystalloid solution. Lid retraction facilitates the irrigation. Alkalis cause more injury than acids because of deep tissue penetration via liquefaction so may need prolonged irrigation (1 to 2 hours). pH of conjunctival sac should be tested and irrigation should be continued until pH is <7.4.and eye protection)
Substance Inhalation
Clear the airway, isolate the airway ASAP meanwhile give high flow oxygen
GI Decontamination
There are several methods of GI decontamination for toxic ingestions; some are very useful/beneficial while others can be harmful.
Forced Emesis – Generally never indicated, as “natural” emesis is just as good as forcing expulsion of gastric contents.
Gastric Lavage
Lavage with a large bore >36 French tube (not just NGT suction with a narrow tube) in order to empty the stomach of toxic contents. Awake patients should be lavaged in left lateral decubitus position to prevent aspiration and facilitate more complete gastric emptying.
Controversial but thought to be potentially helpful if performed within 4 hours of ingestion; preferred if initiated within one hour of ingestion.
Indicated if the airway is protected, removal of toxin is feasible (within a reasonable time frame), and will be beneficial if even a small amount is removed.
Contraindicated for caustic ingestions, large contents unlikely to be removed by lavage, unprotected airway, or timeframe when toxin has probably moved out of the stomach.
Activated Charcoal (AC)
Binds toxins; not indicated for caustics, heavy metals such as lithium, lead, zinc and iron, toxic alcohols, hydrocarbons, and small molecules like sodium, chloride, etc.
Adult dose for unknown exposure is 60 – 90 grams, kids 1g/kg; best if can obtain a ratio of 10:1 of AC:toxin.
No clear timeframe for AC: definite benefit within one hour, suggested benefit within 4 hours; generally no harm in giving for any timeframe if no contraindications exist especially for large ingestions or sustained release preparations.
Contraindicated if absence of gut motility, perforation, risk of aspiration or if endoscopy will be needed; aspirated AC can cause severe pneumonitis.
Whole Bowel Irrigation (WBI)
Instillation of up to 2L per hour (25mL/kg/h for children) of polyethylene glycol solution orally (or via NGT) until the rectal effluent is clear.
Can be used concurrently with AC but may actually compete with toxin for binding sites on AC.
Especially useful for body packers and stuffers.
Caustic Ingestions
Acids – Proton donators, cause injury with pH < 3, hydrogen ions desiccate mucosal cells and cause development of an eschar (coagulative necrosis) that prevents deep penetration.
Can lead to metabolic acidosis with systemic absorption of acids.
Toilet bowl cleaners, hydrofluoric acid, etc.
Alkalis – Proton acceptors, cause injury with pH > 11, hydroxide ions penetrate tissue surfaces and cause liquefactive necrosis until neutralized. Extent of injury is dependent on duration of contact, volume, pH, concentration, penetrating ability of the substance and the TAR (titratable acid or alkaline reserve) – basically the amount of neutralizing substance required to bring the substance to physiologic pH, the higher the TAR the more damaging the substance.
Most household cleaning agents are alkali – ammonium hydroxide (Windex), sodium hypochlorite (bleach), oven cleaners, Drano, detergents etc.
Initial symptoms can be misleading: all patients with stridor or oral lesions require early EGD (within 12-24 hours) in order to accurately diagnose the extent of injury and decrease the risk of iatrogenic perforation.
Combination of multiple symptoms such as drooling, emesis, and chest pain will also likely have high-grade lesions and will need early EGD.
No visible lesions does not mean there is not a high-grade lesion in the esophagus or lower: clinical history and physical exam should guide further investigation.
Initial management should be for decontamination of the patient’s skin and oropharynx as necessary, aggressive control of the airway by direct visualization (consider fiberoptics), and caution with paralytics in severe burns as this may distort airway anatomy with loss of muscular tone.
Consider IV decadron for airway edema.
Gastric decontamination is generally contraindicated unless very early presentation of large volume toxic exposure or with certain high-risk substances as guided by poison control.
Can consider NGT suction for the above if present within 30 minutes; after that there is a very high risk of iatrogenic perforation with NGT so placement should be under direct visualization with EGD.
Initial dilution of liquid caustic ingestions with milk or water may be beneficial but should be discussed with poison control first.
Most patients will require EGD for diagnosis. In the rare patient with late presentation and suspicion of perforation, esophagogram and CT of chest/abdomen are indicated. All high-grade lesions/perforations will require surgical consultation.
***All button batteries lodged in the esophagus require emergent endoscopic removal to prevent perforation***
Antidotes
Dicumarinics - K vitamin
Acetaminophen (paracetamol)- N-acetylcysteine 150 mg/kg dextrose IV over 15–60 min, then 50 mg/kg NAC IV over 4 hrs. Then 100 mg /kg NAC IV over 16 hrs.
Cholinergic (organophosphates, carbamates) Atropine 1-2 mg every 2–3 min, until there is drying of secretions, pralidoxime (2-PAM) 70 mg/kg IV, then infusion at 500 mg/hour
Anticholinesterases Physostigmine 0.5–1 mg IV as a slow push over 5 min and repeated every 10 min
Benzodiazepines Flumazenil 0.2 mg repeated; max dose: 2 mg
β-Blockers Glucagon 3–10 mgCalcium channel blockers Calcium gluconate 10% 10–30 mL IV
Cyanide Amyl nitrite, sodium thiosulfate, sodium nitrite (3% solution), and Vitamin B12
Digoxin Digoxin Fab 5–10 vials
Isoniazid Pyridoxine (vitamin B6) 70 mg/kg IV (maximum 5 g)
Methanol, ethylene glycol Ethanol loading: 8 ml/kg of 10% ethanol then 1–2 ml/kg/hour of 10% ethanol; fomepizole Loading: 15 mg/kg in 100 ml IV over 30 min. Maintenance: 10 mg/kg IV over 30 min every 12 hours for 48 hr.
Narcotics Naloxone 0.1–0.4 mg, may be repeated
Tricyclic antidepressants Sodium bicarbonate 1–2 mEq/kg IV bolus followed by 2 mEq/kg per h IV infusion Iron Deferoxamine IV infusion dose of 15 mg/kg/hour
Methaemoglobinaemia Methylene blue 1–2 mg/kg (0.1–0.2 ml/kg of 1% solution) IV slowly over 5 minLocal anestheticsIntravenous lipid emulsion 1–1.5 ml/kg 20% IV bolus over 1 min, repeat bolus at 3–5 min, then infuse 0.25 ml/kg/min Wernicke’s syndrome, wet beri beri100 mg
IVInsulin, oral hypoglycemics Dextrose (glucose) 1 g/kg IV
Excretion increase
Forced diuresis
Neutral:
No acids or akcaline products, give the patient in 4 hours 500cc of manitol 10% plus 1500 cc of glucosaline serum with 30 mEq of CLK
Acid
Urinary acidification (urine pH below 5.5) with ammonium chloride or ascorbic acid was used in the past to treat toxicity of weak bases such as amphetamines, quinidine, or phencyclidine. However, this practice is not used now because of lack of evidence of efficacy and complications such as iatrogenic toxicity (from severe academia) and rhabdomyolysis may occur.
Alcaline :
Urine alkalinization is a treatment regimen which enhances the elimination of toxins by administration of intravenous sodium bicarbonate to produce urine with pH > or = 7.5.
Alkaline urine acts on ionization of acidotic toxins within renal tubules, stopping resorption of the ionized drug back across the renal tubular epithelium and enhancing elimination through the urine [14].
Useful in salycilates, barbituricsmetotrexate, clorpropamide,diflunsal, acids
1str hour 1000 cc of dextrose 5% + 500 ml HCO3 1/6 M
Next 4 hours 500cc of manitol 10% plus 1500 cc of glucosaline serum with 30 mEq of CLK
General considerations for hemodialysis
Toxin must be very small particles (able to cross the membrane).
Toxin will produce harm if not removed.
Volume of distribution should be small (1L/kg) indicating most of the toxin is in serum.
Toxin should not be highly protein bound (some notable exceptions include aspirin and valproic acid which are almost entirely protein bound at therapeutic levels, but at toxic levels they saturate protein binding sites and the remainder is in serum and therefore dialyzable).
Toxin is unable to be cleared by the body (renal failure, hepatic failure, etc.).
ECMO:
extracorporeal technique used when the patients are critically ill and they cannot provide an adequate amount of gas exchange or perfusion to sustain. This technique may be used in the case of severe and massive overdose especially cardiotoxic drugs (beta blockers, calcium channel blocker) [18].
Disposition
Most of poisoned patients only supportive care with decontamination will be sufficient for them, but antidotes same times is the cornerstone of the treatment.
If the patient has persistent and toxic effects, the patient will require prolonged care course.
Admission is indicated for completing his treatment and observation; in the case of severe toxicity, the patient may need admission to intensive care unit.
In the case of mild toxicity or asymptomatic patient, a 6-hour observation period is sufficient to exclude the development of serious toxicity.
A number of toxins have delayed onset clinical toxicity, for example (but not limited to): modified-release preparations of calcium channel antagonists, selective norepinephrine reuptake inhibitors (tramadol and venlafaxine), and newer antipsychotics (amisulpride); this means that the duration of observation should be longer than usual.
The decision to admit a patient with a toxic exposure to an intensive care setting should be based upon clinical criteria that relate to the stability of the airway, respiratory system, cardiovascular system, and the patient’s level of consciousness.
A retrospective study which was done in more than 200 patients with drug overdoses shows that clinical assessment in the emergency department could reliably find out patients who are at high risk for complications and need intensive care unit admission [19].
Based on the following clinical criteria: if the patient has one of any of the following clinical criteria, the patient may need admission to intensive care unit:
PaCO2 > 45 mmHg
Intubated patient
Seizures post-ingestion
Unresponsiveness to verbal stimuli
Abnormal cardiac rhythm (nonsinus)
Atrioventricular block (Second- or third-degree)
Systolic blood pressure below 80 mmHg
QRS duration ≥0.12 seconds.
REMEMBER TO TREAT THE PATIENT, NOT THE TOXIC
References
– Rosen’s Emergency Medicine – Concepts and Clinical Practice. 8th Edition.
– Goldfrank’s Toxicologic Emergencies 2002.
– An intensive review course in clinical toxicology. New York City Poison Control Center and Bellevue Hospital Center Course Syllabus March 13 and 14; 2014.
– Position paper update: gastric lavage for gastrointestinal decontamination. AACT/EAPCCT. Clin Toxicol. 2013;51:140-146.
– Havanond C, Havanond P. Initial signs and symptoms as prognostic indicators of severe gastrointestinal tract injury due to corrosive ingestion. J Emerg Med. 2007; 33:349-53.
- https://www.intechopen.com/books/poisoning-in-the-modern-world-new-tricks-for-an-old-dog-/general-approach-to-poisoned-patient







































Comentarios